08 September 2025
Anna Ezekiel, 26, is tired but happy. Two days earlier she welcomed her baby boy at Gungu Health Centre in Kigoma Municipal Council where staff have recently completed training in Essential Emergency and Critical Care (EECC). The facility is also equipped with lifesaving tools to identify and manage critical illness. Although she had a normal delivery, Anna suffered from severe bleeding (postpartum haemorrhage) a complication which was identified early due to the new routines introduced as part of EECC. A nurse monitoring Anna’s vital signs noticed the increasing pulse rate, acted swiftly and gave her iv fluids to prevent shock, allowing time to stop the cause of bleeding and transfusing blood.
“I am very happy with the service I received. The staff have been monitoring me closely and I feel much better. I hope to be able to go home soon,” Anna says with relief.
 A nurse showing UNICEF Health specialist Anase Minja the chart where Anna’s vital signs and EECC treatments were documented.
A nurse showing UNICEF Health specialist Anase Minja the chart where Anna’s vital signs and EECC treatments were documented.
In just the past month, Anna is one of four women to battle the life-threatening dangers of postpartum haemorrhage at Gungu Health Centre.
“We deliver up to 300 babies here every month and often manage mothers with serious complications. In the past, by the time I was called to help, these mothers were usually already in a critical state, and many needed referrals to the regional hospital, but following the introduction of EECC, this has changed,” says Dr Diana Adam, the council’s EECC coordinator and clinician in the health centre, with a proud smile on her face.

EECC is transforming care for critically ill patients across Tanzania through a collaboration between UNICEF, Muhimbili University of Health and Allied Sciences, Ministry of Health and President’s Office for Regional Administration and Local Government, with funding from Global Affairs Canada via the CanGive Initiative.
EECC makes the difference between uncertainty and a peaceful start to motherhood.
“Recently, I attended to three mothers with PPH where the nurse had already taken appropriate action. Vital signs – breathing, oxygen saturation, blood pressure and pulse – had been checked and treatments began immediately, following EECC protocols. None of these mothers needed referral, and they could all leave the health centre healthy,” says Dr Diana.
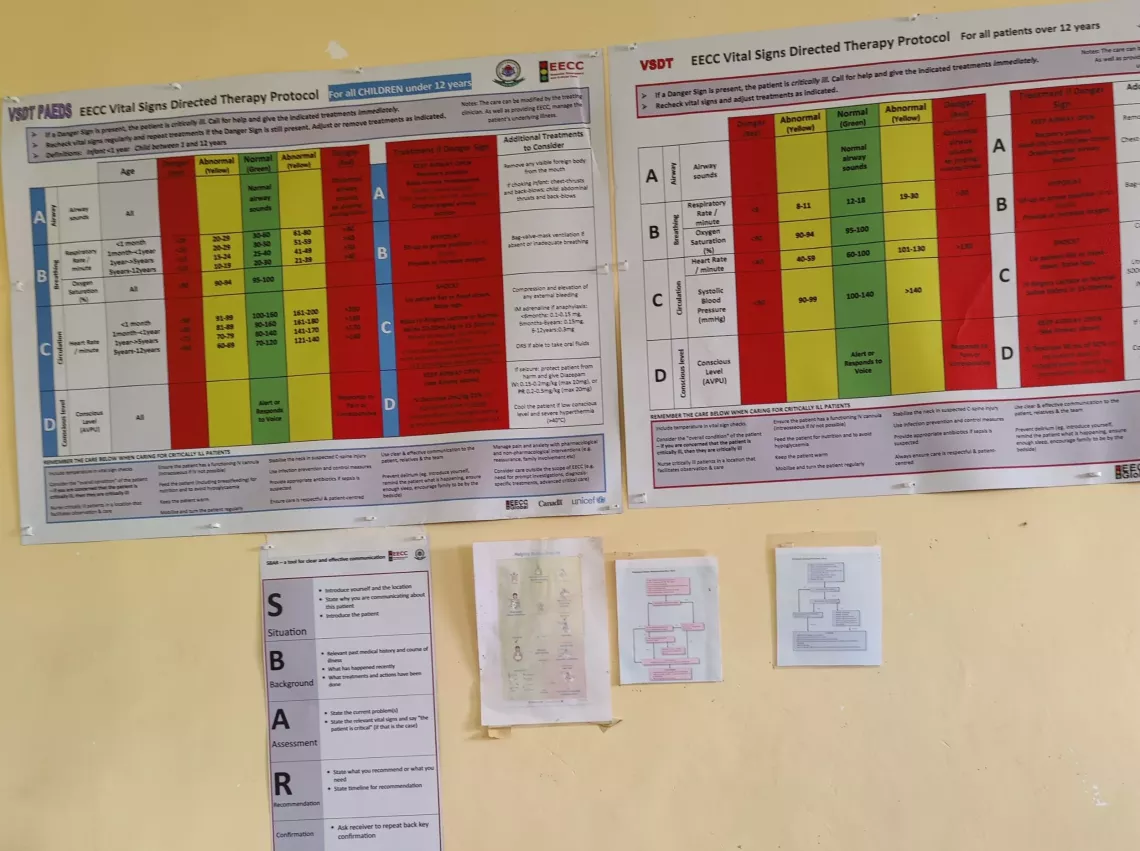 EECC protocols displayed in the maternity unit.
EECC protocols displayed in the maternity unit.